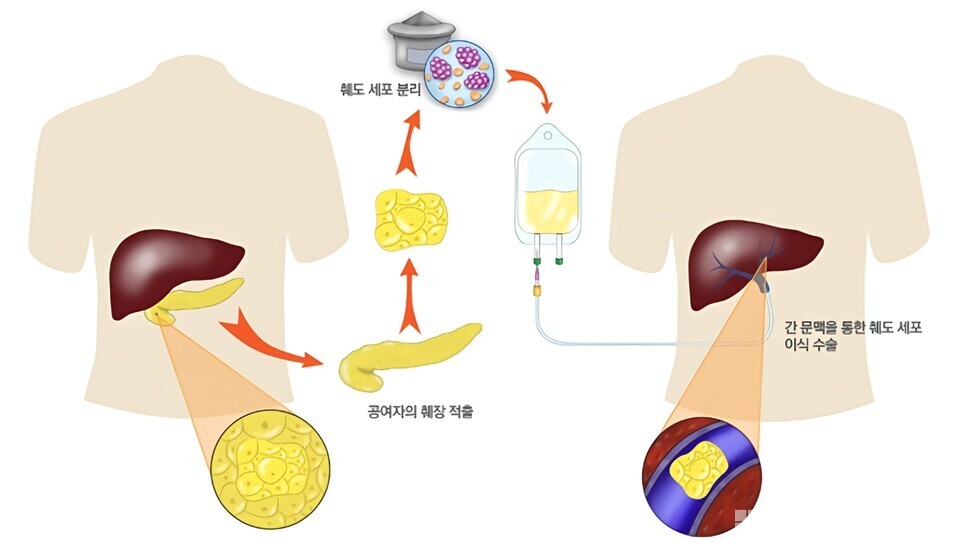
Type 1 diabetes is an autoimmune disease where the insulin production is halted as the beta cells in the pancreas are destroyed by the immune system. One of the most effective current treatments is islet transplantation, but issues such as donor shortages, decreased survival rates of transplanted cells, and immune rejection remain unresolved. However, a new cell transplantation technique has recently emerged, offering the potential to overcome these limitations.
According to a study published in Science Advances, researchers have successfully reversed Type 1 diabetes in mice through subcutaneous transplantation using vascularized islets. Unlike traditional islet transplantation methods relying on portal vein administration, this study achieved stable glucose control through a safer and simpler subcutaneous approach.
The biggest hurdle for previous islet transplantation was the failure to secure adequate vascular supply. Islets require a vascular network to function normally, but in the traditional method, the process of vascular formation often resulted in cell damage or loss of function. To address this, the researchers pre-vascularized the islets using reprogrammed vascular endothelial cells (R-VECs) before transplantation.
The key to this technology is utilizing R-VECs, which temporarily express the vascular-specific transcription factor ETV2, to induce the formation of an intrinsic vascular network within the islets. The study found that the vascularized islets maintained the function of secreting insulin in response to glucose and formed normal blood flow, enhancing survival even after subcutaneous transplantation.
Currently, most islet transplants are performed via the portal vein. However, liver-based transplants come with surgical risks and a high likelihood of immune response damaging the transplanted cells. In contrast, subcutaneous transplantation has advantages such as lesser surgical burden, easier monitoring, and ease of graft removal if necessary. Despite these benefits, the success rate of conventional subcutaneous transplantation was low due to difficulties in vascular formation.
By using vascularized islets containing R-VECs, the study established functional blood flow in the subcutaneous region through successful connection with host vasculature. The R-VECs formed vascular networks which were larger in diameter (13.5 ± 7.5μm) than the capillaries of human pancreases, suggesting improved blood flow.
In diabetic model mice, the transplantation of vascularized islets under the skin normalized hyperglycemia. Human insulin levels were significantly detectable in the recipient’s serum after transplantation, and hyperglycemia reappeared upon removal of the graft, verifying that the transplanted vascularized islets were managing diabetes through insulin production.
Traditionally, the major concern with islet transplantation has been immune rejection, necessitating lifelong immunosuppressive therapy with potential side effects. However, the vascularized transplantation method used in this study shows promise in enhancing cell survival while minimizing immune rejection. Researchers highlighted the need for further research to reduce immune response without conventional immunosuppressants.
This research could potentially redefine Type 1 diabetes treatment. If subcutaneous transplantation becomes viable, more patients could achieve insulin independence safely. Researchers aim to move towards clinical trials, potentially establishing a practical treatment for humans.
If commercialized, this technology might allow Type 1 diabetes patients to maintain normal blood glucose levels with a single transplant, obviating the need for lifelong insulin injections.
The medical community is closely observing whether this new approach will revolutionize islet transplantation therapy and emerge as a breakthrough in diabetes treatment.